Model-informed dosing in pregnancy
Absorption, distribution, metabolism & excretion
Absorption
During pregnancy, stomach acidity decreases and the production of the hormone progesterone increases. Lower stomach acidity reduces the absorption of basic drugs (drugs with a high pH) while it increases the absorption of acidic drugs (drugs with a lower pH). Progesterone causes smooth muscle cells in the gastrointestinal tract to relax. This slows down gastric emptying and gut movements. Consequently, drugs are absorbed more slowly. On the other hand, the cardiac output (the amount of blood the heart pumps through the body per minute) increases during pregnancy. Because of this, more blood is pumped towards the intestines. This, in turn, enhances the absorption of drugs. In addition, many women experience nausea and vomiting in early pregnancy. This may decrease the amount of drug available for absorption, especially following oral intake.
Overall, the effect of pregnancy on absorption is drug-specific. However, taken together, the effects of pregnancy on drug absorption are likely to be minimal as pregnancy-induced changes in the gastrointestinal system that reduce drug absorption are compensated by the increase in cardiac output.
Distribution
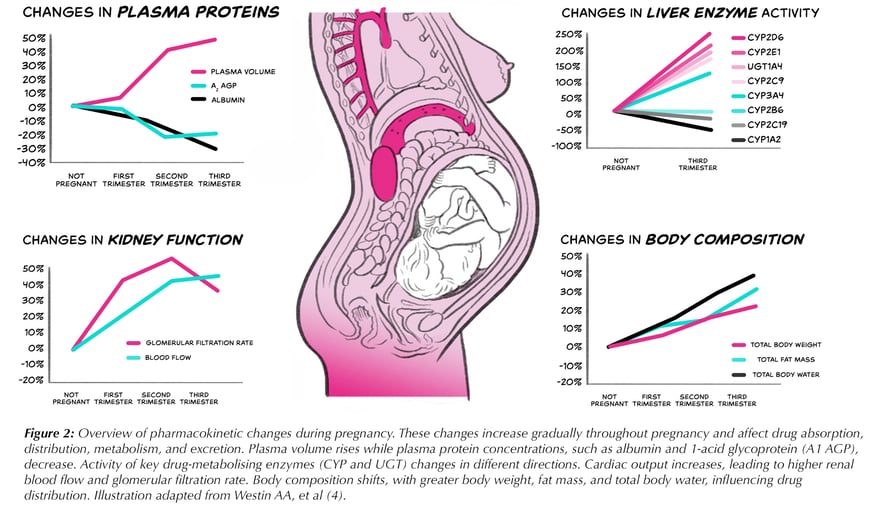
The amount of blood, body water and body fat significantly increases during pregnancy. This causes drugs to spread differently in the body and causes changes in the volume of distribution of a drug. The volume of distribution of a drug is a measure of how extensively it spreads across the body. The a drug’s volume of distribution depends on its physical and chemical characteristics. Drugs can either be lipophilic (repelled by water and attracted to fat) or hydrophilic (favouring water and repelled by fat). With more body water in pregnancy, hydrophilic drugs dilute into a larger space, often producing lower peak blood concentrations and sometimes a longer half-life. Similarly, increased fat stores can expand the Vd for lipophilic drugs.
Also, changes in plasma proteins during pregnancy can impact drug distribution. Due to the increasing blood volume in pregnancy, the concentration of proteins circulating in the bloodstream decreases. An example of a plasma protein that shows a decrease in concentration during pregnancy is albumin. With fewer binding proteins, a larger proportion of the drug remains unbound. These changes can impact the volume of distribution and potentially the effects of a drug, especially if the unbound drug distributes poorly into tissues or is cleared slowly.
Overall, due to a higher volume of fluids in the body, pregnancy often leads to lower peak concentrations of drugs in the bloodstream. This may lead to lower efficacy for certain drugs.
Metabolism
Metabolism, drug breakdown, enables elimination via urine or faeces and is carried out primarily by liver cytochrome P450 (CYP) enzymes, though other enzymes can also be involved. Pregnancy hormones, such as progesterone and oestradiol, change the abundance and activity of these enzymes, some increase, others decrease. Liver blood flow also rises, further influencing metabolism. As a result, some drugs are broken down faster, lowering plasma levels, while others are metabolized more slowly, increasing plasma levels.
Overall, The effect depends on the specific enzymes involved for each drug.
Elimination
Alongside drug metabolism by liver enzymes, the kidneys play an important role in removing drugs from the body. Because of an increased cardiac output in pregnancy, there is an increased blood flow to the kidneys. This change starts in the second trimester and continues during the third trimester of pregnancy. In addition, due to the increase of unbound drug in the bloodstream during pregnancy, drugs that are filtered by the kidneys are removed from the body more quickly during pregnancy. Faster renal filtration results in an increased drug clearance. On top of renal filtration, the kidneys contain small channels (‘tubules’) that can reabsorb drugs from urine as well as secrete drugs into urine. Renal absorption and secretion are also influenced by hormonal changes as part of pregnancy. This may impact the speed of drug removal from the body.
Overall, drugs tend to be removed faster from the body during pregnancy. This is mainly a result of increased renal filtration. These changes can result in a shorter duration of therapeutic levels of the drug in the body during pregnancy.
